Introduction
- Multiple sclerosis is an autoimmune disease characterized by inflammation, selected demyelination, and gliosis.
- It causes both acute and chronic symptoms, disability, and impaired quality of life.
Etiology
Genetic
Risk of multiple sclerosis is increased in persons with an affected family member.
The risk is 3% for a sibling, 5% for fraternal twins, and 25% for identical twins.
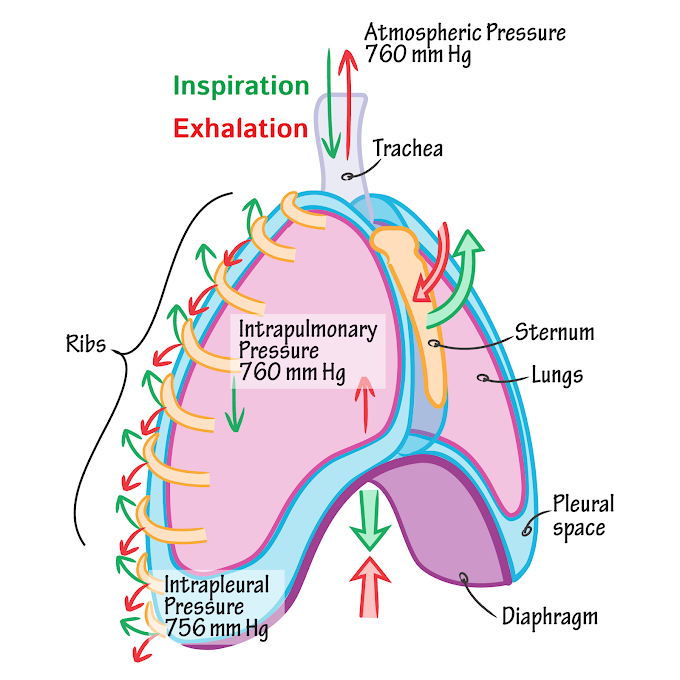
 |
| Fig.1: Etiology of multiple sclerosis |
Immunological factors
When persons with genetic susceptibility are exposed to the viral agent, the immune system response with activated myelin-active lymphocyte, called molecular mimicry.
This abnormal immune response causes inflammation and damage to the Central Nervous System.
Molecular mimicry is similarities between foreign and self-peptides are sufficient to result in cross-activation of T or B cells by pathogen-derived peptides.
Infective Factors
Measles, Human herpes virus-6, Epstein-Barr virus (EBV), and Chlamydia pneumonia, Canine distemper.
Vitamin D
People who live near the equator are exposed to a greater amount of sunlight they have a higher level of naturally produced vitamin D.
vitamin D helps in to support immune function and may help in to protect against immune-mediated diseases like multiple sclerosis.
Risk of multiple sclerosis may also be increased with vitamin D deficiency.
Smoking
Many studies suggest that stopping smoking (before or after the onset of multiple sclerosis) is associated with a slower progression of disability.
Pathophysiology
- In patients with multiple sclerosis, the immune responses trigger activation of immune cells such as T and B cells, CD4+ helper T-cells that cross the blood-brain barrier.
- These cells activate autoantigens that produce an auto-immune cytotoxic effect within the central nervous system (CNS).
- 👉👉 Phagocytic activity of macrophages May contributes to the demyelination of neurons.
- An acute inflammatory event occurs.
- Edema and infiltrates (e.g., monocytes, macrophages, and microglia) surround the acute lesion and cause abnormally increased pressure that further interfere with the conductivity of nerve fibers.
- During, the early stage of multiple sclerosis oligodendrocytes survive and produce remyelination.
- As the disease becomes chronic the oligodendrocytes become involved and myelin repair cannot occur.
- Demyelinated areas are filled with fibrous astrocytes and undergo a process called gliosis.
- Gliosis is a proliferation of neuroglial tissue within the central nervous system and results in glial scars (Plaque).
- This is the main cause of permanent neurological disability.
Symptoms of Multiple Sclerosis
Symptoms of multiple sclerosis depend on the location of specific lesions.
1. Sensory Symptoms
- Hypoesthesia: a decreased sense of touch or sensation.
- Numbness of face, body, or extremities
- Paresthesia: means altered sensation
2. Pain
- 55% of patients with multiple sclerosis experience pain clinically.
- Patient's experience acute, paroxysmal pain characterized by sudden and spontaneous onset.
- Pains are described as intense, sharp, shooting, electric shock-like, and burning.
- Common types of pain:
- Paroxysmal limb pain
- Headache
- Optic or trigeminal neuritis
- Lhermitte's sign: In patients with posterior column damage, flexion of the neck produces electric shock-like sensation running down the spine to lower extremities.
- Hyperpathia: hypersensitivity to minor sensory stimuli.
- Chronic neuropathic pain: result from the demyelinating lesion in spinothalamic tracts or in the sensory roots.
3. Visual Symptoms
- Optic neuritis: inflammation of the optic nerve that produces an ice pick-like pain behind the eye with blurring or greying of vision or blindness in one eye.
- Scotoma: dark spot maybe occurs in the centre of the visual field.
- Nystagmus:
- The involuntary cyclical movement of the eyeball (horizontal or vertical) that develop when the patient looks to the sides or vertically (gaze-induced nystagmus) or when the patient moves the head.
- A result from lesions affecting the cerebellum or central vestibular pathways.
- Lateral gaze palsy:
- Internuclear ophthalmoplegia produces incomplete eye adduction (lateral gaze palsy) on the affected side and nystagmus of the opposite abducting eye with gaze to one side.
- It is caused by demyelination of the medial longitudinal fasciculus.
- Diplopia
4. Motor Symptoms
Patients with corticospinal lesions demonstrate signs and symptoms of upper motor neuron syndrome such as;
- Paresis or weakness of muscle
- Spasticity
- Brisk tendon reflexes
- Involuntary flexor and extensor spasm
- Clonus
- Positive Babinski's sign
- Exaggerated cutaneous reflexes
- Loss of autonomic control
 |
| Fig.1: Areas affected by multiple sclerosis |
5. Fatigue:
A subjective lake of physical and mental energy that is perceived by the individual to interfere with usual and desired activities.
6. Coordination and balance
A demyelinating lesion in the cerebellum and cerebellar tracts producers cerebellar symptoms such as:
- Ataxia: uncoordinated movements.
- Postural tremor
- Intention (action) tremor: involuntary, rhythmic, shaking movements occur when purposeful movement is attempted.
- Hypotonia
- Truncal weakness
- Impaired gait
7. Speech and Swallowing
- Dysarthria: slurred or poorly articulated speech with low volume, unnatural emphasis, and slow rate.
- Dysphonia: change in vocal quality including harshness, hoarseness, breathiness, or hypernasal sounds.
- Dysphagia: poor coordination of the tongue oral muscles can result in difficulty in swallowing.
8. Short-term memory loss
9. Depression
10. Anxiety
11. Emotional
- Pseudobulbar affect:
- also known as Involuntary emotional expression disorder/Emotional incontinence.
- It is characterized by sudden and unpredictable episodes of crying, laughing, or other emotional display.
- Euphoria consists of an exaggerated feeling of well being.
- Bipolar affective disorder
12. Bladder and Bowel Symptoms
- Demyelinating lesions affect the lateral and posterior spinal tracts unmasked the sacral reflex arc producing a loss in volitional and synergistic control of the micturition reflex.
- Type of bladder dysfunction in MS
- Flaccid bladder
- Spastic bladder
- Dyssynergic bladder: problem with coordination between the bladder contraction and sphincter relaxation.
- Constipation is the most common bowel complaints in MS and results from legends affecting control of gastrocolic reflex.
13. Sexual Dysfunction
- Sexual dysfunction affects 91% of men and 72% of women.
- In women, symptoms can include:
- Changes in sensation
- Vaginal dryness
- Trouble reaching orgasm
- Loss of libido (sexual desire).
- In men, symptoms can include:
- Importance
- Decreased sensation
- Difficulty or inability to ejaculate
- Loss of libido.
Disease Course
Multiple sclerosis is highly variable and unpredictable from person to person.
Benign Multiple Sclerosis
- Disease in which the patient remains fully functional in all neurological systems 15 years after onset.
Malignant Multiple Sclerosis/Marburg Disease
- It is a rare disease course characterized by rapid onset and progression leading to disability or death within a short time after onset.
There is 4 major clinical course
1. Relapsing-Remitting Multiple Sclerosis (RRMS)
- Characterized by separate attacks of neurological deficit (relapse) followed by partial or full recovery (remission) in certain weeks to months.
- Periods between relapses are characterized by a lack of disease progression.
- The stable patient may have a local inflammatory activity that is clinically silent.
- RRMS affects approximately 85% of patients with multiple sclerosis at diagnosis.
 |
| Fig. 1: RRMS |
2. Secondary Progressive Multiple Sclerosis (SPMS)
- Characterized by an initial relapsing-remitting course followed by a change in clinical course with progression to steady and irreversible decline with or without continued acute attacks.
- May be the result of progressive axonal loss rather than new lesions.
- 90% of cases of RRMS are progressed to SPMS in 25 years.
 |
| Fig. 2: SPMS |
3. Primary-Progressive Multiple Sclerosis (PPMS)
- Characterized by continuous worsening of the disease from the onset.
- Patients may experience fluctuations in neurological disability but distinct attacks do not occur.
- PPMS is associated with letter onset (mean age 40 years) and more equal gender distribution.
- PPMS affects approximately 10% of patients with multiple sclerosis.
 |
| Fig. 3: SPMS |
4. Progressive-Relapsing Multiple Sclerosis (PRMS)
- Characterized by study deterioration in disease from onset (similar to PPMS) but with occasional acute attacks.
- Intervals between attacks are characterized by continuing disease progression.
- PRMS affects approximately 5% of patients with multiple sclerosis.
Diagnosis of Multiple Sclerosis
Neurophysiological Tests: may detect asymptomatic lesions.
Visual evoked potential (VEP)
Somatosensory evoked potential (SSEP): may detect Central sensory pathway lesions.
Brain stem auditory evoked potential (BAEP): may detect brainstem lesions.
Cerebrospinal Fluid Examination: patients with multiple sclerosis show elevated total immunoglobulin (IgG) in CSF and the presence of oligoclonal IgG bands in response to inflammatory demyelinating lesions.
MRI: is highly sensitive to detecting MS plaques in the white matter of the brain and spinal cord.
Medical Management of Multiple Sclerosis
Medications are used to help treat and prevent relapses (exacerbation) and slow the progression of neurological disability and also given to provide symptom relief.
Management of Acute Relapses
- Corticosteroid therapy is used to treat acute disease relapses (exacerbation), shortening the duration of the episode.
- These drugs show:
- Powerful anti-inflammatory effects
- Immunosuppressive effects
- Diminished swelling within the central nervous system (CNS)
- Decreased T-cell activation
- Limited immune cell penetration of the CNS, and
- Enhance the apoptosis of activated immune cells.
Management of Symptoms
Pharmacological agents are used for symptomatic relief in MS.
- Spasticity
Drugs that act at spinal or muscle level-
- Baclofen (GABA derivative)
- Dantrolene (direct act on muscle)
- Tizanidine (alpha-2 adrenergic agonist)
- Urinary symptoms
Incomplete bladder emptying-
Intermittent self-catheterisation
Dextrusor instability-
Anticholinergics
Desmopressin spray
- Bowel symptoms
Lactulose
Loperamide (increase anal sphincter tone)
- Pain
Analgesics
Anticonvulsants
Antidepressants
NSAIDs
TENS
- Paroxysmal symptoms
e.g. tonic seizure – anticonvulsants
- Fatigue
Amantadine
Modafinil
- Tremor/ataxia
Beta-blockers
Primidone
Buspirone
Physical Therapy Management
- Management of Sensory Deficits and Skincare
- Management of Fatigue
- Management of Pain
- Exercise Training
- Management of Spasticity
- Gait Training & Functional Training
- Management of Speech & Dysphagia
- Cognitive Training
Related Topics:
- Physiotherapy Management of MS
- Physical examination of MS patient
- Parkinson's disease
References:
- Davisplus.fadavis.com
- aan.com
- Physical Rehabilitation by Susan B. O'Sullivan




0 Comments