Introduction
- Vestibular rehabilitation (VR), or vestibular rehabilitation therapy (VRT) is a specialized form of therapy intended to alleviate both the primary and secondary problems caused by vestibular disorders.
- VR is an exercise-based program primarily designed to reduce vertigo and dizziness, gaze instability, and/or imbalance and falls.
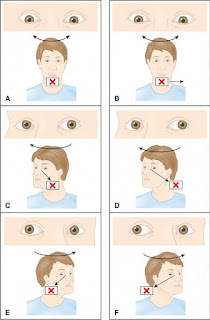
 |
| Fig.1: Vestibular rehabilitation |
Contraindications of Vestibular Rehabilitation
- Vestibular rehabilitation is not appropriate for the unstable vestibular disorder (e.g., Ménière's disease, uncontrolled migraine, PLF, or unrepaired superior semicircular canal dehiscence).
- Therapist's alert to:
- Sudden loss of hearing
- Increased feeling of pressure or fullness to the point of discomfort in one or both ears
- Severe ringing in one or both ears.
- The therapist must be observant for the discharge of fluid from the ears on the nose, which may indicate CSF fluid leak.
- Patients with acute neck injuries may not be able to tolerate physical examination, CRM, gaze stability exercises.
Interventions for Benign Paroxysmal Positional Vertigo (BPPV)
- Three different treatment approaches have been developed on the basis of the pathophysiology of the BPPV.
- The techniques include the canalith repositioning maneuver, Liberatory (semont) maneuver, and Brandt–Daroff exercises.
Canalith Repositioning Maneuver (CRM)
- Also known as the Epley maneuver.
- Based on the canalithiasis theory of free-floating otoconia in the semicircular canal.
- The patient's head is moved into different positions in a sequence that will move the otoconia out of the involved semicircular canal and into the vestibule.
- Once the otoconia are in the vestibule, the sign and symptoms should resolve.
- The positions used in the treatment of posterior and anterior semicircular canal canalithiasis can be the same.
- The procedure of CRM:
- The patient's head is first rotated 45° toward the involved side.
- The patient is then moved into the Dix-hallpike position with the affected left ear toward the ground.
- Next, the head is rotated 90° to the right and maintains the 30° extension during this step. The head should now be positioned 45° to the right.
- The patient is rolled onto the right shoulder and slowly brought up to the sitting position, head still rotated at 45° to the right.
Between each step, the therapist should wait for 1 to 2 minutes or until vertigo and nystagmus have stopped to ensure otoconia flow through the canal.
Liberatory (Semont) Maneuver
- Treatment for posterior semicircular canal BPPV based on cupulolithiasis theory.
- It involves rapidly moving the patient through positions designed to dislodge the otoconia from the cupula.
- Liberatory Maneuver or right posterior SCC BPPV:
- The head is rotated 45° to the left side.
- With assistance, the patient is then moved from the setting to the right sideline and stays in this position for 1 minute.
- The patient is then rapidly moved 180°, from right side-lying to left side-lying. That should be in the original starting position, left rotated (nose down in the final position).
- After one minute in this position, the patient returned to sitting.
Brandt–Daroff Exercises
- Exercises are designed to habituate the CNS to the provoking position.
- They may also act to dislodge otoconia from the cupula or by causing otoconia to move out of the canal.
- Exercises for posterior SCC BPPV:
- The patient starts in a sitting position and turns the head 45° to one side (left) then quickly lies down on the opposite shoulder (right). The patient should be instructed to remain in this position for 30 seconds or until the vertigo stops.
- The patient then slowly returns to the starting position, maintaining the head rotation (left) until sitting upright.
- The patient turns the head to the opposite direction (right) and nice down on the other shoulder (left), absorbing the similar 30 second time guidelines.
- The exercise should be done 10 to 20 times, three times per day until the patient is without vertigo for two consecutive days.
Goals of BPPV Interventions:
- The otoconia will be returned into the vestibule.
- The patient will demonstrate reduced vertigo associated with head motion.
- The patient will demonstrate improved balance.
- The patient will demonstrate independence in a daily activity involving head motion.
Interventions of Unilateral Vestibular Hypofunction (UVH)
1. Gaze Stability Exercises
- The purpose of these exercises is to improve the VOR and other systems that are used to assess the stability with head motion.
- Vestibular adaptation exercises are designed to expose patients to retinal slip.
- A retinal slip occurs when the image of an object moves off the fovea of the retina resulting in visual blurring.
- The two primary exercises of vestibular adaptation are:
- Exercise 1:
- The patient is asked to move the head horizontally and vertically as quickly as possible while maintaining focus on a stable target.
- A good target to use is a business card, asking the patient to focus on a word or a letter within a word.
- Exercise 2
- The patient is asked to move the head and target in opposite directions while focusing on the target.
- Increasing the difficulty by the use of varying the distance from which the patient performs the exercises, moving the head more rapidly, and performing the exercise while standing or walking.
- The computerized DVA test is useful to improve gaze stability for individuals with UVH and TBI.
2. Postural Stability Exercises
- The purpose of postural stability exercises is to improve balance by encouraging the development of balanced strategies.
- The table shows Balance Exercises and Progression.
3. Habituation Exercises
- Habituation Exercises are prescripted when a patient with a UVH has continual complaints of dizziness.
- Habituation is defined as a deduction in response to a repeatedly performed movement.
- To determine which habituation exercise to be prescribed, the physical therapist must determine the provoking positions first.
- When a position elicits mild to moderate dizziness, the patient remains in the provoking position for 30 seconds or until symptoms are gone.
- The patient is provided with the home exercise program based on the results of the positional test.
- The exercises are designed to reduce dizziness and the patient should be encouraged that the symptoms normally decrease within two weeks.
- If after two weeks the symptoms are no better, the habitation exercises should first be changed.
- If this is not helpful then the patient should be referred to either a physical therapist with special training in vestibular rehabilitation or a physician for further evaluation.
Goals of Interventions:
- The patient will demonstrate improved stability of gaze during head movement.
- The patient will demonstrate diminished sensitivity to motion.
- The patient will demonstrate improved static and dynamic postural stability.
- The patient will be independent in the proper performance of a home exercise program that includes walking.
👉👉Patients with UVH should be informed that recovery time after initiating vestibular rehabilitation is 6 to 8 weeks.
Interventions for Bilateral Vestibular Hypofunction (BVH)
1. Gaze stability exercises
- Use of exercise 2, is not recommended for a patient with a BVH because this exercise may cause an excessive retinal slip.
- But in patients with asymmetrical BVH, exercise 2 is useful.
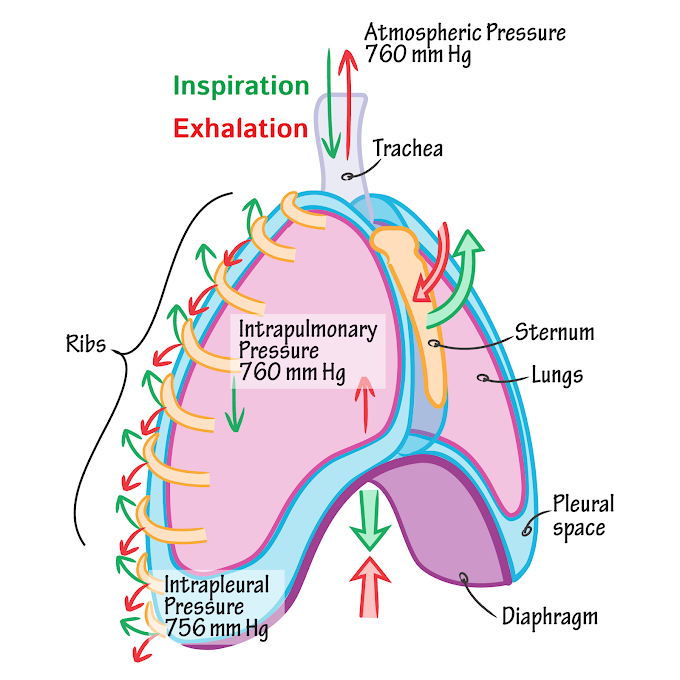
 |
| Fig.1: Gaze stability exercises |
2. Postural stability exercises.
3. Habituation exercises.
Goals of Interventions:
- The patient will demonstrate improved stability of gaze during head movement.
- The patient will demonstrate reduced subjective complaints of gaze instability.
- The patient will demonstrate improved static and dynamic balance.
- The patient will be independent in the proper performance of a home exercise program (HEP) that includes walking.
- The patient will demonstrate enhanced decision-making skills regarding the performance of basic and instrumental activities of daily living.
Interventions for Abnormal Central Vestibular Function
- Goals of intervention:
- The patient will demonstrate enhanced decision-making skills regarding fall preventions and safety precautions to allow safe functioning within the home and community.
- The patient will demonstrate enhanced decision-making skills regarding the use of compensatory strategies to assist in gaze stability.
- The patient will be independent in the performance of a HEP that includes walking.
- The physical therapy intervention for a central vestibular lesion at a level of brainstem likely will be similar to a UVH with the same expectations for recovery.
- Gait and balance exercises
- Habituation exercises
References:
- Physical Rehabilitation by Susan B. O'Sullivan
Related Topics:
- Vestibular Disorder
- Examination of a patient with vestibular disorder



0 Comments