MUSCLES OF RESPIRATION
Primary Muscles
- Responsible for changing the thoracic cage during normal or quiet breathing.
Accessory Muscles
- They are to help the primary muscle during forceful breathing.
- Inspiratory Muscles
- Primary muscle:
- Diaphragm muscle
- External Intercostal muscle
- Accessory muscle:
- Sternocleidomastoid muscle
- Scalene
- Pectorals
- Anterior serratus
- Elevators of scapula
- Expiratory muscles
- Primary muscle:
- Internal intercostal muscle
- Accessory muscle:
- Abdominal muscle
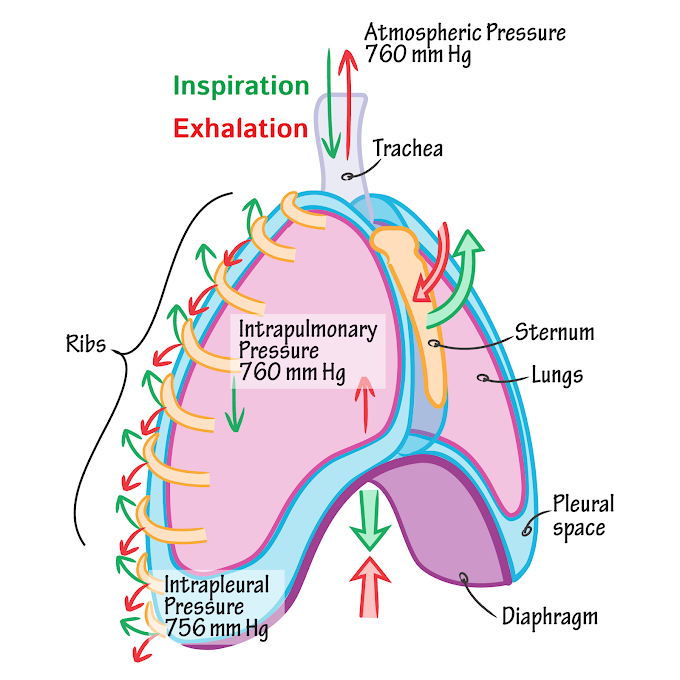
RESPIRATORY PRESSURES
Intra-alveolar pressure or Intra-pulmonary pressures: are the pressure existing in the alveoli of the lungs
Intrapleural pressure or Intrathoracic pressures: are the pressure present in the pleural cavity i.e. between the visceral and parietal layer of the pleura. these pressure are negative
Atmospheric pressure: pressure on the surface of the chest. It is considered as zero
Transmural pressure: are pressure across the wall of the structure
TRANSMURAL PRESSURE = (Pressures inside the wall) - (Pressure outside the wall)
 |
| Fig.1: Respiratory pressures |
Transmural pressure can be;
- Positive----- pressure responsible for inflating the lung
- Negative-----responsible for deflating the lung
- Zero-----no net inflating or deflating pressure
TYPES OF TRANSMURAL PRESSURE:
- Transpulmonary pressure:
- is the pressure across the alveoli
- = (intra-alveolar pressure) - (intrapleural pressure)
- Transpulmonary pressure determine How much inflating or deflating pressure on the lung
- Transthoracic pressure:
- is the pressure across the chest wall
- = (Pleural pressure) - (Atmospheric pressure)
- Trans respiratory pressure:
- = (Alveolar pressure) - (Atmospheric pressure)
LUNG VOLUMES AND CAPACITIES
LUNG VOLUMES
Lung volumes are also known as respiratory volumes. It refers to the volume of gas in the lungs at a given time during the respiratory cycle.
1. Tidal volume(TV)
It is the amount of air which move in & out of the lung during quiet inspiration & quiet expiration
The normal adult value is 500mL
2. Inspiratory Reserve Volume(IRV)
It is an extra volume of air that can be inspired forcefully by the help of accessory inspiratory muscle after the end of normal inspiration.
The normal adult value is 3300mL.
3. Expiratory Reserve Volume(ERV)
It is an extra volume of air that can be expelled out forcefully after a normal expiration.
The normal value is 1000mL.
4. Residual Volume(RV)
It is the volume of air remaining in the lung even after forced expiration
The normal value is 1200mL.
LUNG CAPACITIES
Lung capacities are derived from a summation of different lung volumes.
1. Functional Residual Capacity(FRC)
It is the volume of air remaining in the lung after a normal tidal expiration.
FRC = RV + RRV
=1000mL+1200mL
=2200mL
=2.2L
2. Vital capacity(VC)
It is the maximum volume of air that can be exhaled out forcefully after a forceful inspiration.
VC = ERV + TV + IRV
=1000mL+500mL+3300mL
=4800mL
3. Inspiratory Capacity(IC)
It is the maximum volume of air that is inspired after a normal expiration.
IC = TV + IRV
=500mL+3300mL
=3800mL
4. Total Lung Capacity(TLC)
It is the volume of air present in the lung after forceful inspiration.
TLC = RV + ERV + TV + IRV
=1200mL+1000mL+500mL+3300mL
=6000mL
=6L
SURFACE TENSION
Alveoli are lined by 2 different epithelial cells,
1.Type I pneumocyte:
Type I pneumocytes are flat cells
They cover around 95% of the entire surface area of alveoli
They provide an excellent space for gas exchange.
2. Type II pneumocyte:
Type II pneumocytes are cuboidal cells
they produce surfactant, that decreases the surface tension
So, the Surface tension is the force imposed by water molecules at the air-liquid interface & acts to minimize the surface area of alveoli.
COMPLICATIONS OF INCREASED SURFACE TENSION
Tendency of Alveolar collapsing: surface tension leads to a reduction in the surface area & it is making alveolar smaller that increases the collapsing tendency. Due to surface tension, there is collapsing pressure in alveoli.
The tendency of Edema: if surface tension is increased too much then it pulls the water from the pulmonary capillary by simple diffusion in the alveoli. Alveoli is loaded with water that increases the thickness of the alveolar membrane, so thicker membranes can not participate in gas exchange.
Collapsing of smaller alveoli: Laplace’ Law states that pressure in a sphere being directly proportional to twice the surface tension and inversely proportional to the radius:
P=2T/r
P= collapsing pressure
T surface tension
r= radius of alveoli
We have two spheres with different sizes. As the radius of the sphere decreases, the pressure increases as per Laplace's Law. Now, If the two spheres were connected with a tube, the smaller one should empty into the larger one based on the pressure difference. In other terms, smaller alveoli should empty into larger ones based on Laplace's law, causing the lungs to collapse.
Compliance
- Compliance is the ability of the lung & chest wall to expend or it is the expandability of the lung and chest wall.
- The compliance of a lung is also defined as the change in volume per unit change in the pressure of the lung.
Lung Compliance (C) = Change in Lung Volume (V) / Change in Transpulmonary Pressure (P)
Types of Compliance
Q. why during inspiration lungs are less compliant and why during expiration lung are more compliant
- This difference shows that when the lung is smaller, it is difficult to expand by increasing the pressure.
- At residual volume, lung size is small and alveoli are also smaller
- Alveoli are filled with fluid secreted by type 1 pneumocytes that have strong intermolecular forces & the lung is stiffened.
- When inspiration starts then intra-alveolar pressure is increased, which is initially required for the breakdown of intermolecular forces & stickiness of alveoli.
- As inspiration continues, the smaller alveoli become larger and the intermolecular force becomes weaker.
- When the lung reaches at End inspiratory volume or at total lung capacity then the lung is fully expended and intermolecular forces become less.
- During Expiration, the intra alveolar pressure is decreases and intermolecular force increasing
- So, at specific pressure lung is less compliant during Inspiration & more compliant during Expiration.




0 Comments