History of Patient
Symptoms:
- Dizziness is a sense of disturbed relationship between oneself and one's environment.
- Vertigo is defined as an illusion of movement.
- Lightheadedness is defined as a feeling that fainting is about to occur.
- Dysequilibrium is defined as the sensation of being off-balance.
- Oscillopsia is a subjective experience of the motion of objects in the visual environment that is known to be stationary (Table 1).
Duration of Symptoms
- Determine how recently the patient has had acute attacks of vertigo, lightheadedness, dysequilibrium, or oscillopsia.
- Determine the symptoms are constant or episodic.
- If the symptom is episodic then determine the average duration of episodes in seconds, minutes, or hours.
- For example:
- Vertigo lasting seconds to minutes commonly suggest benign paroxysmal positional vertigo.
- Vertigo lasting minutes to hours suggest Méniére's disease.
- Vertigo lasting 4 days implies vestibular neuronitis and migraine-associated dizziness.
- Determine under what circumstances the patient experiences symptoms.
Special Tests:
1. Visual Analogue Scale:
- The use of VAS is an effective technique to obtain subjective intensity ratings of vertigo, lightheadedness, dysequilibrium, and oscillopsia (e.g., How intense are your symptoms).
2. Examination of Eye Movements:
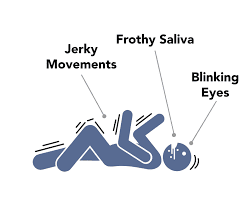
1. Observation for Nystagmus
- Nystagmus is an involuntary eye movement, due to peripheral vestibular lesion and composed of both slow and fast components.
- In the patient with unilateral vestibular lesion, the slow component is due to relative excitation of one side of the vestibular system and the first component is generated from the para pontine reticular formation in the brainstem and repositions the eye to the center of the orbit.
- For example in the left beating nystagmus, the eyes move slowly to the right (vestibulo-ocular reflex), and the resetting eye moment is to the left (fast component).
- Spontaneous nystagmus may always be present in the dark after the unilateral loss of vestibular function.
- Vestibular nystagmus can be suppressed in light and when a person visually fixates on a target.
- Observation of nystagmus should be performed under conditions in which the person cannot see. Which is achieved by Frenzel lenses (Fig.1) or an infrared camera system.
- Frenzel lenses look like large goggles with magnifying lenses that enable the clinician to observe for nystagmus while preventing the patient from fixating on a target, and an infrared camera uses infrared light to illuminate the eyes while the patient remains in complete darkness.

Fig.1: Frenzel lens.
2. Head Impulse Test (HIT)
- The head impulse test is used to examine a semicircular canal function.
- Cervical ROM should be determined before performing the head impulse test and the physical therapist should explain why the head must be moved quickly.
- Impulse test is performed by having the patient first fixate on a near target (e.g., the clinician's nose).
- When testing the horizontal semicircular canal, the head is flexed 30°.
- Patients asked to keep their eyes focused on a target while their head is manually rotated in an unpredictable direction using a small amplitude, moderate velocity, and high acceleration angular impulse.
- When the vestibular ocular reflex is functioning normally, the eyes move in the opposite direction to the head movement and the gaze will remain on the target.
- In a patient with loss of vestibular function, the vestibulo-ocular reflex will not move the eyes as quickly as the head rotation and eyes move off the target. The patient will then make a corrective saccade to reposition the eyes on the target.
- A corrective saccade is a rapid eye movement used to reposition the eyes to the target.
- The appearance of corrective saccades indicates vestibular hypofunction as determined by the head impulse test and occurs because of inhibition of vestibular afferents and central vestibular neurons on the Intact side (persons with unilateral vestibular hypofunction).
- A patient with a bilateral loss of vestibular function will make corrective saccades after a head impulse to either side.
- The head impulse test provides a sensitive indication of vestibular hypofunction in patients with complete loss of function in the affected labyrinth.
- This test is less sensitive in detecting the type of function in patients with incomplete loss of function.
3. Head-Shaking Induced Nystagmus Test
- The head-shaking induced nystagmus (HSN) test is useful in the diagnosis of unilateral peripheral vestibular defects.
- During this test, vision is occluded.
- The clinician flexes the head 30° before oscillating horizontally for 20 cycles at a frequency of 2 repetitions per second.
- On stopping the oscillation, the patient opens the eyes and the clinicians check for nystagmus.
- In normal vestibular function, nystagmus will not be present.
- The asymmetry between the peripheral vestibular inputs to central vestibular nuclei may result in head shaking induced nystagmus.
- A person with unilateral vestibular hypofunction will manifest a horizontal HSN.
- Patients with a complete loss of vestibular function bilaterally will not have HSN because neither system is functioning, so there is no asymmetry between the tonic firing rates.
- The presence of vertical nystagmus after either horizontal or vertical head-shaking suggests a central lesion.
4. Positional Testing
- Positional testing is commonly used to identify whether otoconia (crystal) have been displaced into the semicircular canal, causing a condition called benign paroxysmal positional vertigo (BPPV).
- The addition of otoconia into the endolymph makes the semicircular canals sensitive to changes in head position.
- Dix-Hallpike test
- The most common positional test used to examine the posterior semicircular canal BPPV.
- The patient is moved from a long sitting position with the head rotated 45° to one side, to a supine position with the head extended 30° beyond horizontal, head still rotated 45°.
- The maneuver places each of the semicircular canals in a gravity-dependent position and the therapist should observe the eyes for nystagmus.
- The direction of nystagmus is unique to the involved semicircular canal.
- The direction and duration of the resultant nystagmus can help determine whether the patient has BPPV or a central lesion.
- It is used to examine horizontal semicircular canal BPPV.
- The patient is positioned supine with the head flexed 20 degree
- Rapid rotation to the side is done separately and the clinician observed for nystagmus and vertigo.
5. Dynamic Visual Acuity Test
- Dynamic visual acuity is the measurement of visual activity during horizontal motion of the head.
- The head velocities need to be greater than 100°/sec at the time dynamic visual acuity is measured.
- To perform the test, static visual acuity is determined first.
- The patient is asked to "read the lowest line you can see" on a wall-mounted acuity chart.
- The wall chart is recommended because they provide uniform light illuminance for each of the letters.
- The patient then attempts to read the chart while the clinician horizontally oscillates the patient's head at s frequency of 2 Hz.
- Metronome is used to ensure the correct frequency of oscillation.
- For patients with loss of vestibular function the eyes will not be stable in space during head movements.
- This causes a decrement in DVA compared with static visual acuity.
- Using the acuity chart, 3-line or more decrement in visual acuity during head movement is suggestive for vestibular hypofunction.
- Computerized DVA has been found to correctly identify the side of lesions in patients with unilateral hypofunction for self-generated and unpredictable head motion and can be used to identify single semicircular canal lesions.
3. Examination of Gait and Balance:
- Examination of gait and balance is important for the determination of the patient's functional status.
- Testing should address both static and dynamic balance.
- gait and balance tests cannot uniquely identify pathology within the vestibular system.
- Table 2, includes common balance tests and expected results.
4. Vestibular Function Tests
Semicircular Canals Tests
- Semicircular canal test includes electro-nystagmography (ENG)
- ENG is a battery of tests that measure oculomotor, inner ear function, and nystagmus in different head positions.
- ENG test includes:
- Caloric Test
- Infusion of cold and warm water into the external auditory canal with the help of a syringe so that it touches the tympanic membrane.
- This stimulus introduces a temperature gradient which results in the convective flow of endolymph that deflects the cupula and generates nystagmus from the horizontal semicircular canal.
- Rotational Chair Test
- This test stimulates each semicircular canal by rotating the patient in the dark.
- In patients with normal vestibular function, nystagmus should be generated by rotation.
- In the presence of vestibular disorder, the pathology can be determined by comparing VOR gain and phase from rotation toward one ear with rotations towards the opposite ear.
- The rotational chair test is the standard test for bilateral vestibular hypofunction.
Otolith Tests
- Vestibular-Evoked Myogenic potential (VEMP) Test
- VEMP uses the threshold and amplitude of a muscle contraction (EMG) to classify pathology.
- VEMP includes:
- Cervical VEMP
- Ocular VEMP
References: Physical Rehabilitation by Susan B. O'Sullivan



0 Comments