Vestibular Disorder
- If a disease or injury damages the vestibular system, then you can have a vestibular disorder.
 |
| Fig.1: Vertigo, dizziness |
Types of Vestibular Disorder
- Peripheral vestibular disorder
- Benign paroxysmal positional vertigo (BPPV)
- Unilateral Vestibular Hypofunction (UVH)
- Bilateral Vestibular Hypofunction (BVH)
- Ménière's Disease
- Perilymphatic Fistula
- Vestibular Schwannoma
- Central vestibular disorder
- Vertebrobasilar Ischemic Stroke
- Vertebrobasilar Insufficiency (VBI)
- Multiple Sclerosis
- Migraine-Related Dizziness
- Cervicogenic Dizziness
Peripheral Vestibular Disorder
- Patients with a peripheral disorder demonstrate nystagmus to the contralateral side which suppresses with visual fixation.
- Common peripheral Vestibular disorder are:
1. Benign paroxysmal positional vertigo (BPPV)
- BPPV is a biomechanical disorder
- Symptoms:
- Nystagmus
- Vertigo with a change in head position
- Nausea with or without vomiting
- Dysequilibrium
- Latency to the onset of vertigo and nystagmus occurs within 15 seconds, once the head is in the provoking position.
- The duration of symptoms is usually less than 60 seconds.
Pathophysiology:
- Vertigo and nystagmus are caused by the misplaced otoconia (crystal).
- Mechanisms: Cupulolithiasis and Canalithiasis, both theories involve the otoliths becoming dislodged from the utricle and falling into the semicircular canals.
- Cupulolithiasis:
- The fragments of otoconia break away and adhere to the cupula of one of the semicircular canals (Fig.1 A).
- When the head is more into certain positions, the weighted cupula is deflected by the pull of gravity.
- This abnormal signal results in vertigo and nystagmus, which persists as long as the patient is in the provoking position.

Fig.1: (A) Canalithiasis (B) Cupulothiasis - Canalithiasis:
- The otoconia are floating freely in one of the semicircular canals (Fig.1 B).
- When a patient changes head position, the pull of gravity causes the freely floating otoconia to move inside the semicircular canal resulting in endolymph movement and deflection of the cupula.
2. Unilateral Vestibular Hypofunction (UVH)
- Causes: decreased receptor input, which is the result of viral insults, trauma, and vascular events.
- Symptoms:
- Vertigo
- Spontaneous nystagmus
- Oscillopsia during head movements
- Postural instability
- Dysequilibrium.
- Initially, the patient will experience vertigo and nystagmus impairment due to the asymmetry in tonic firing rates, created when one vestibular system is no longer functioning.
- Spontaneous horizontal nystagmus usually resolves within 3 to 7 days in patients with UVH.
- Persistent symptoms of vertigo beyond two weeks should be considered chronic and also necessitating vestibular rehabilitation.
3. Bilateral Vestibular Hypofunction (BVH)
- Causes:
- Meningitis
- Auto-immune disease
- Head trauma
- Ototoxicity (most common)
- Tumors on each 8th cranial nerves
- Transient ischemic episodes
- Sequential unilateral Vestibular neuronitis
- Symptoms:
- Dysequilibrium
- Oscillopsia
- Gait ataxia
- Postural instability
- Decreased visual acuity with head movement
- Reduced VOR gains
- Unless the BVH is asymmetrical, the patient will not experience nausea, vertigo, or nystagmus because there is no asymmetry in the tonic firing rate of the vestibular neurons.
4. Ménière's Disease
- Symptoms:
- Low-frequency hearing loss,
- Episodic vertigo,
- Sense of fullness in-ear,
- Tinnitus.
- Symptoms gradually increase in severity and can last several hours per episode.
- During an episode, vestibular exercises are not recommended.
- Chronic Ménière's disease can result in UVH, for which vestibular rehabilitation is appropriate.
- Pathophysiology: increase in endolymphatic pressure (due to increase in endolymphatic fluid) resulting in inappropriate nerve excitation which gives rise to the symptoms.
- Dietary restriction for self-treatment is less sodium intake (2g/day), avoid caffeine and alcohol.
- Physical therapy is also useful in the treatment of dysequilibrium occurring after a vestibular neurectomy or chemical ablation.
5. Perilymphatic Fistula
- Perilymphatic fistula (PLF) is the most common cause by a rupture of an oval around Windows, membranes that separate the middle and inner ear.
- Rupture of these membranes result in leakage of the paralympic into the middle ear and result in vertigo and hearing loss.
- Causes:
- Trauma
- Excessive pressure changes (e.g., deep water diving)
- Blunt head trauma without skull fracture
- Extremely loud noise
- Patients are treated first with bed-rest allowing the membrane to heal and then surgical patches of fistula are performed.
- Physical therapy is contraindicated for most patients with the PLF.
- But it can be beneficial for those patients who have continual dysequilibrium or develop a vestibular hypofunction postoperatively.
6. Vestibular Schwannoma
- Vestibular Schwannomas are also known as acoustic neuromas.
- It is a benign tumor arising from the Schwann cell of the 8th cranial nerve, in the internal auditory canal (IAC).
- The IAC also contains the facial nerve (7th CN) and internal auditory artery along with the vestibulocochlear nerve (8th CN).
- Symptoms:
- Tinnitus
- Hearing loss
- 👉Both are initial symptoms
- Vertigo (vestibular hypofunction)
- Imbalance
- Facial symptoms
- Vascular symptoms
- Treatment: surgical excision of the tumor.
- On tumor removal, most unilateral vestibular afference is lost and the brain now perceives asymmetrical vestibular input.
- Physical therapy is initiated during the early postoperative period to resolve symptoms of dysequilibrium and oscillopsia.
Central Vestibular Disorder
1. Vertebrobasilar Ischemic Stroke
- The blood supply to the brainstem, cerebellum, and inner ear is derived from the vertebrobasilar system.
- Occlusion of any of the major branches [anterior inferior cerebellar artery (AICA), posterior inferior cerebellar artery (PICA), and vertebral artery] may result in vertigo.
- Causes:
- Atherosclerosis
- Embolism
- Vertebral artery dissection
- Subclavian steal syndrome
- Hypercoagulation disorder
- Inflammatory conditions.
- The symptoms associated with ischemic stroke are dependent upon which branch of the system is occluded.
- Occlusion of Posterior Inferior Cerebellar Artery (PICA) will cause Lateral Medullary Infarction and result in Wallenberg's syndrome/lateral Medullary syndrome and characterized by:
- Vertigo
- Nystagmus
- Gait disturbance
- Ipsilateral limb ataxia
- Facial pain or numbness
- Contralateral body hemianesthesia
- Horner's syndrome
- Dysphagia
- Hoarseness
- Facial nerve paralysis
- Occlusion of Anterior Inferior Cerebellar Artery (AICA) will cause lateral pontomedullary infarction and result in lateral inferior pontine syndrome.
- This syndrome is characterized by symptoms similar to Wallenberg's syndrome.
- Involvement of 8th & 7th cranial nerves results in ipsilateral facial paralysis and tinnitus and hearing loss.
- Dysphagia and hoarseness, however, are not apparent as 9th and 10th cranial nerve nuclei are uninvolved with occlusion of the anterior inferior cerebellar artery.
- Occlusion of the vertebral artery may affect the cerebellum only. Sign and symptoms are:
- Mimic a peripheral vestibular hypofunction.
- Dysdiadochokinesia
- Past pointing (inability to place a finger or some other part of the body accurately on a selected point).
- Patients with transient ischemic attack may present with sudden vertigo that last minutes and complaint of hearing loss.
- Atherosclerosis
- Embolism
- Vertebral artery dissection
- Subclavian steal syndrome
- Hypercoagulation disorder
- Inflammatory conditions.
- Occlusion of Posterior Inferior Cerebellar Artery (PICA) will cause Lateral Medullary Infarction and result in Wallenberg's syndrome/lateral Medullary syndrome and characterized by:
- Vertigo
- Nystagmus
- Gait disturbance
- Ipsilateral limb ataxia
- Facial pain or numbness
- Contralateral body hemianesthesia
- Horner's syndrome
- Dysphagia
- Hoarseness
- Facial nerve paralysis
- Occlusion of Anterior Inferior Cerebellar Artery (AICA) will cause lateral pontomedullary infarction and result in lateral inferior pontine syndrome.
- This syndrome is characterized by symptoms similar to Wallenberg's syndrome.
- Involvement of 8th & 7th cranial nerves results in ipsilateral facial paralysis and tinnitus and hearing loss.
- Dysphagia and hoarseness, however, are not apparent as 9th and 10th cranial nerve nuclei are uninvolved with occlusion of the anterior inferior cerebellar artery.
- Occlusion of the vertebral artery may affect the cerebellum only. Sign and symptoms are:
- Mimic a peripheral vestibular hypofunction.
- Dysdiadochokinesia
- Past pointing (inability to place a finger or some other part of the body accurately on a selected point).
2. Vertebrobasilar Insufficiency (VBI)
- Vertebrobasilar insufficiency is synonymous with a transient ischemic attack (TIA) of the vertebrobasilar system.
- The symptoms resolve within 24 hours.
- If left untreated, the disease process will progress to stroke with permanent or long-lasting consequences.
- Causes:
- Motor vehicle accident (MVA)
- Cervical spondylosis
- Symptoms:
- Visual field cuts [loss of peripheral vision (Hemianopia)]
- Visual dysfunction
- Drop attacks (sudden, spontaneous falls)
- Incoordination
- Symptoms may last from minutes to hours in duration.
- Motor vehicle accident (MVA)
- Cervical spondylosis
- Visual field cuts [loss of peripheral vision (Hemianopia)]
- Visual dysfunction
- Drop attacks (sudden, spontaneous falls)
- Incoordination
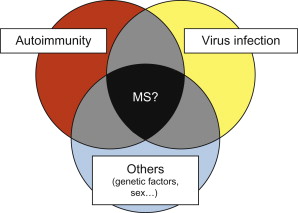
3. Multiple Sclerosis
- MS can affect the 8th cranial nerve where it enters the brainstem.
- Sign and symptoms are identical to unilateral vestibular hypofunction (UVH).
- Diagnosis: MRI
4. Migraine-Related Dizziness
- Migraine related symptoms include:
- Vertigo,
- Dizziness,
- Imbalance, and
- Motion sickness.
- A recent study reported 100% of migraineur's head abnormal nystagmus during a migraine episode if they were positionally tested as a part of the oculomotor examination.
- Vestibular rehabilitation in patients with migraines can be very helpful but patients with both vestibular hypofunction and migraine do not respond as well.
- Vertigo,
- Dizziness,
- Imbalance, and
- Motion sickness.




0 Comments